After Surgery
Sternal Precautions
• Not have much of an appetite. It takes several weeks for your normal appetite to return. Many patients notice that their sense of taste initially is diminished or almost absent. Don’t worry, it will return. Some patients even are nauseated by the smell of food for a week or two after surgery.
• Have some swelling, especially if you have a leg incision. Your leg may continue to swell for some time. Elevate your legs, do your exercises, and wear your compression/support hose, if prescribed. These things will help with the swelling.
• Have difficulty sleeping at night. You may find it difficult to fall asleep, or you may wake up at 2:00 a.m. or 3:00 a.m. and not be able to fall back to sleep. This will improve. If difficulty sleeping or staying asleep is due to pain or significant discomfort, taking your prescribed pain medication about an hour before bed may help. Also, exercising during the day will help you fall asleep faster and sleep more soundly.
• Have problems with constipation. You may use a stool softener or laxative of your choice. Drinking plenty of water and walking, as approved by your doctor, and adding more fruits, vegetables, fiber, and juice in your diet will help move things along.
• Have mood swings and feel sad on some days. Your body went through some major changes during surgery. Don’t become discouraged. This will get better as your body continues to heal. Talk to your doctor if you experience feelings of anxiety or depression.
• Have a lump at the top of your incision. If it is tender and slightly pink or red, this is normal and should disappear with time. Contact your doctor if you notice increased swelling, redness, or pain.
• Notice an occasional clicking noise or sensation in your chest in the first days after surgery. This should occur less often with time and go away completely within the first couple of weeks. If it gets worse, call your surgeon.
• Experience muscle pain or tightness in your chest, shoulders, and upper back between your shoulder blades. This will improve with time. Your pain medicine also will help relieve this discomfort. If the pain increases, call your surgeon or 911.
Medications
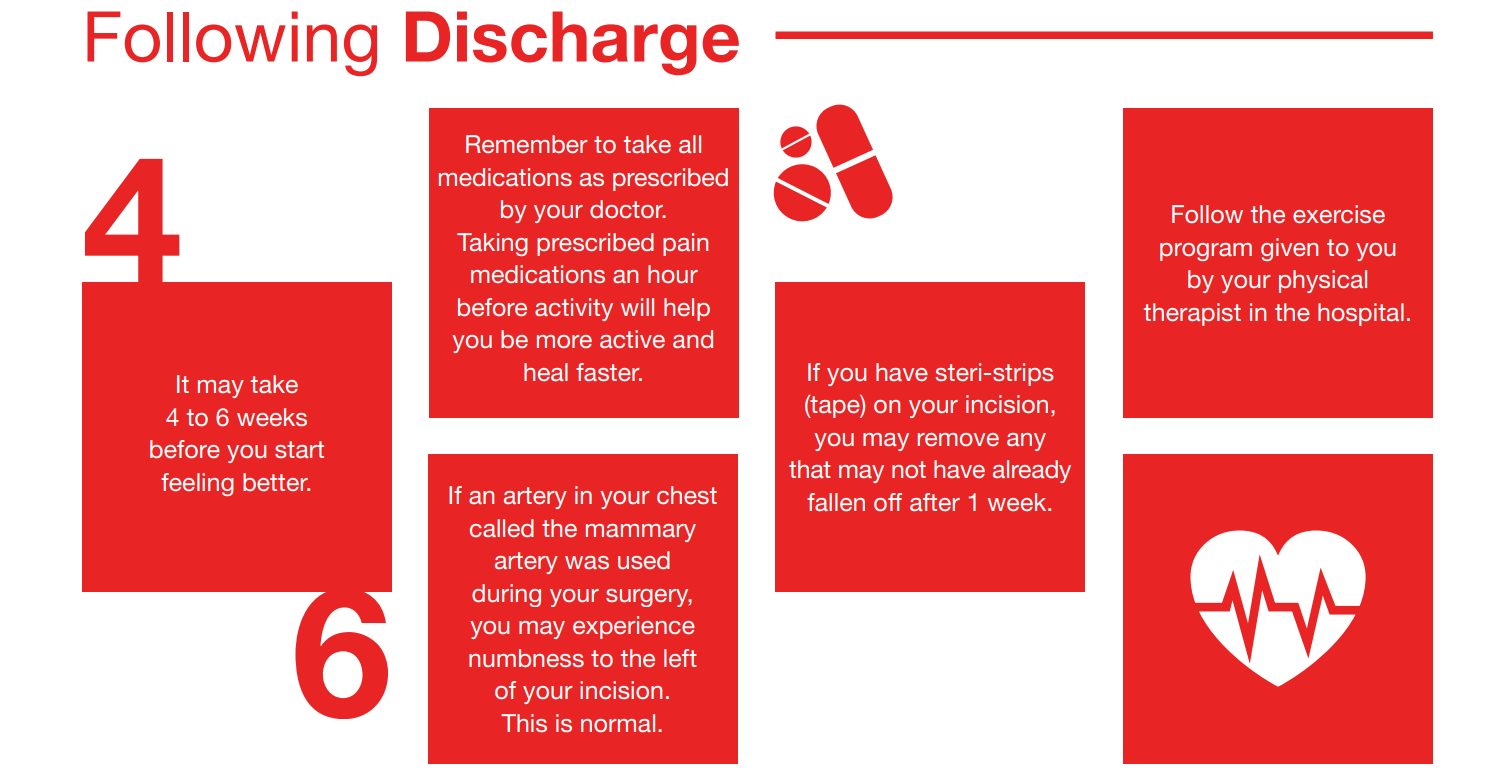
Your doctor will prescribe medications when you are discharged from the hospital. Sometimes these medications will be sent electronically to your pharmacy, or you will receive a paper prescription. It is important to have your insurance cards with you when you pick up your prescriptions at the pharmacy.
Take the medicine exactly as your doctor prescribes. Keep a current list of your medicines, dosages, and times to be taken in your wallet or purse. Do not take other medication, supplements, or herbal preparations without telling your doctor. Additional information about your medications will be provided by your nurse or pharmacist before discharge.
SIDE EFFECTS
It is important to understand that medications can cause side effects. Take them with a small meal, if appropriate. If you have any of the following side effects from medication, you should call your doctor’s office:
- Diarrhea, constipation, or stomach pain
- Nausea, vomiting, and upset stomach
- Dizziness or lightheadedness when standing
- Confusion
- Tingling in hands and feet
- Extremely slow or fast pulse
- Skin rash
- Unusual bruising or bleeding
+ Heart Surgery Discharge +
Call the clinical nurse
specialist/case manager with
questions related to:
- Helpful community services or agencies
- Incisional care
- Postoperative recovery
- Discharge instructions
- Home health care
- Surgery
- Draining or reddened wounds
- Management of symptoms
What your doctor/nurse might
ask if you call:
- How long have you had these symptoms?
- What medications are you currently taking and when did you last take them?
- When did you have surgery?
- Who was your surgeon?
- Where was your surgery done?
- What was the date of your hospital discharge?
- Does the visiting nurse come to see you?
- What about incisional drainage? What is the drainage color; does it have an odor; how long has it been draining; is the drainage getting better or worse; is the area red and/or swollen?
Showers: You can take showers after your pacing wires and staples are out. Avoid soaking in baths until your incisions are healed. Avoid extremely hot water.
Dress: Wear comfortable, loose-fitting clothes that do not put undue pressure on your incisions. If you wear a bra, choose one without underwires and with a front closure.
Rest: You need a balance of rest and exercise during your recovery. Plan to rest between activities and take short naps as necessary. Resting also includes sitting quietly for 20-30 minutes. After meals, rest for 30 minutes before exercising.
Walking: This is one of the best forms of exercise because it increases circulation throughout the body and to the heart muscle. It is important to increase your activity gradually. Walk at your own pace. If you get tired, stop and rest.
Each person progresses at a different rate after heart surgery. Before your discharge, physical therapists will provide you with an individual plan for exercise. It is important to pace your activities throughout the day. Do not try to do too many things at one time. When the outside temperatures are lower than 40°F or above 80°F, walk at indoor shopping malls. In colder weather, wear a scarf or mask around your mouth and nose.
Stairs: Unless your doctor tells you differently, you can climb stairs. Take them at a slow pace. Stop and rest if you tire. When using the handrail, do not pull yourself up with your arms. Use your legs.
Sex: You can resume sexual relations when you feel comfortable. For many people, this is about 2-4 weeks after discharge, unless instructed differently by your doctor. Ask your nurse for more detailed information, if needed.
Driving: You can ride as a passenger in a car at any time. Always wear a seat belt. You may not drive if you are taking narcotics. You may only drive if you are capable of operating the vehicle safely at all times, especially important is being able to brake and check blind spots. When traveling, be sure to get out of the car every 2 hours and walk around for a few minutes.
Lifting: You should not put too much strain on your sternum while it is healing. Avoid lifting, pushing, or pulling anything heavier than 10 pounds for 6 weeks after surgery. After the 6 weeks, you may add up to 20 pounds per week to your carrying capacity. Speak to your doctor if you experience weakness after 6 weeks.
This includes carrying children, groceries, and suitcases, as well as mowing the grass, vacuuming, and moving furniture. Don’t hold your breath during any activity, especially when lifting anything or when using the restroom.
Work: Most patients will begin to feel like returning to light work 6-12 weeks after surgery. Check with your surgeon and get cleared before returning to work.
Visitors: Limit your visitors for the first couple of weeks. If you get tired, excuse yourself and lie down. Your visitors will understand.
When To Resume Normal Activities
DIET
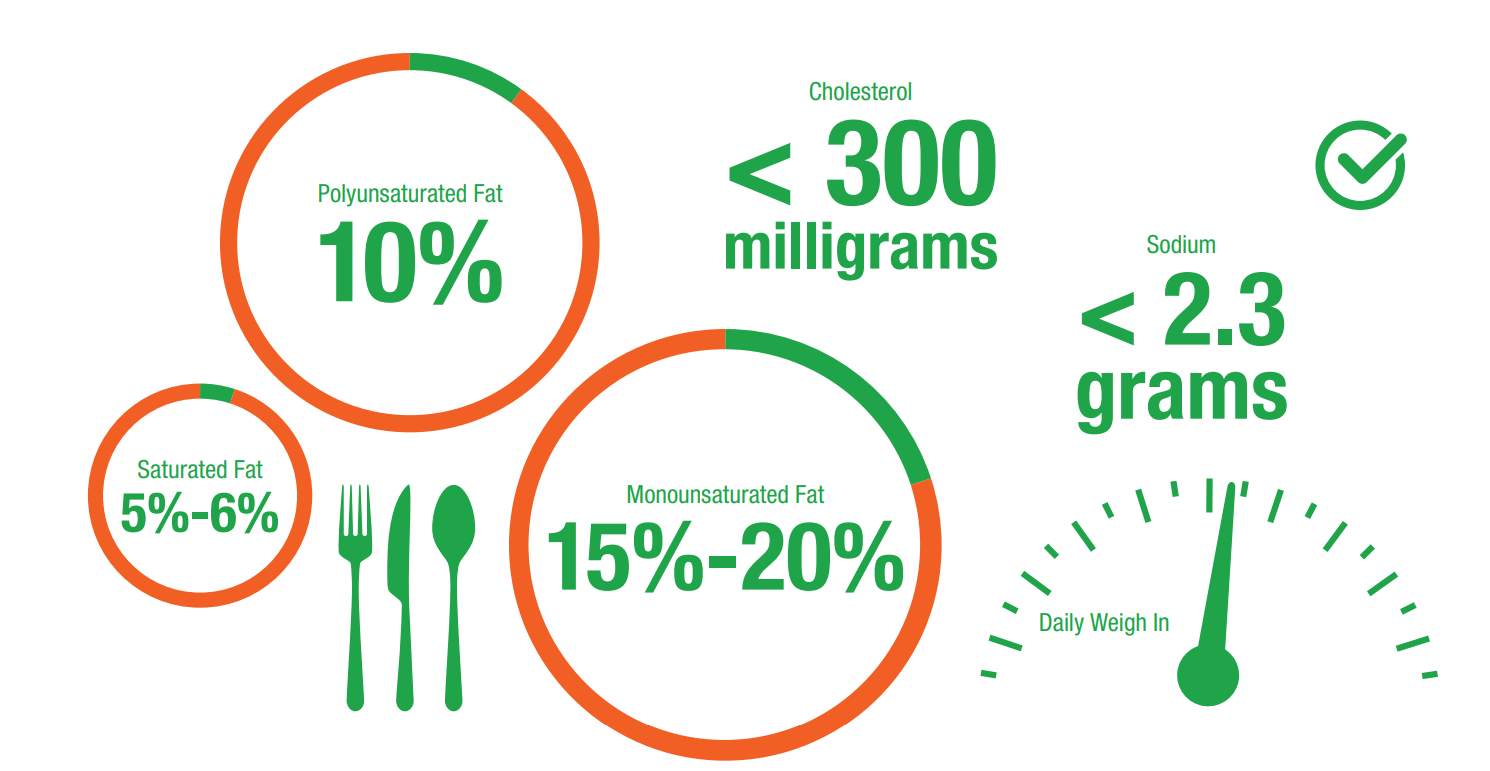
After discharge, your doctor will recommend that you follow a low-fat diet and that you avoid adding salt when cooking or at the table. This may reduce your risk of a future heart attack and your need for another angioplasty or surgery. You should try to have less than 30% of your calories from fat. It also is recommended that you eat less saturated fat and cholesterol.
The American Heart Association suggests:
- Saturated fat intake should be 5%-6% of calories
- Polyunsaturated fat intake should be up to 10% of calories
- Monounsaturated fat should be approximately 15%-20% of total calories
- Cholesterol intake should be less than 300 milligrams per day
- Sodium intake should be no more than 2,300 milligrams (2.3 grams) per day
Review your medication instructions for any possible dietary interactions. You should begin making changes to your diet when your appetite returns to normal.